This website is intended for US healthcare professionals.
Could cardiovascular (CV) inflammation be a silent perpetrator behind CV events?1
What is CV inflammation?
CV inflammation is an inflammatory response that, if unaddressed, can contribute to plaque destabilization and CV conditions like atherosclerosis and heart failure.2
What is inflammatory CV risk?
Inflammatory CV risk is the risk indicated by high-sensitivity C-reactive protein (hsCRP) levels ≥2 mg/L and is commonly referred to in literature as ‘inflammatory risk’.1,3
Uncovering evidence:
CV inflammation is an independent driver of major adverse cardiovascular events (MACE)1,4
An observational study of 84,399 adults showed:

~60% of patients with atherosclerotic cardiovascular disease (ASCVD) have inflammation (indicated by hsCRP ≥2 mg/L) and therefore remain at risk for major CV events, even after accounting for traditional CV risk factors4
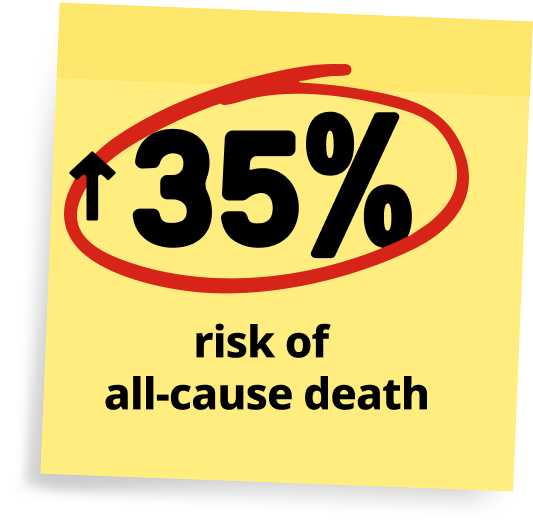
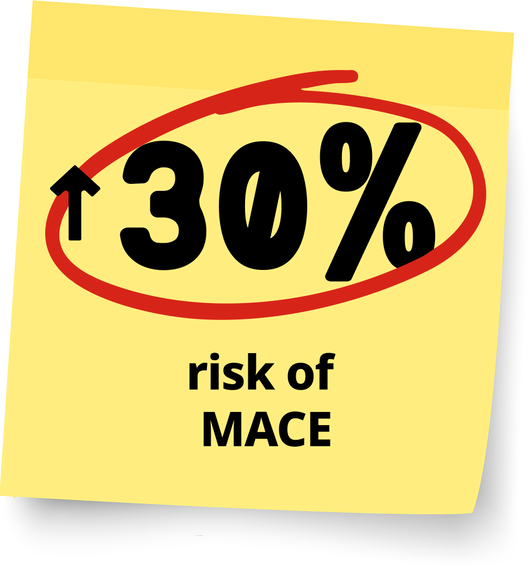
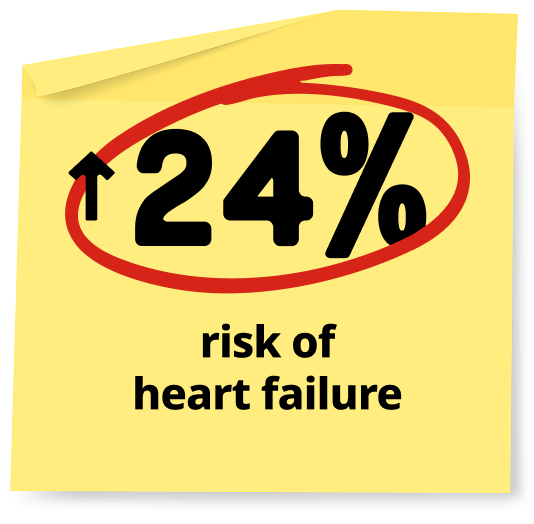
CV inflammation in adults with ASCVD can signal a rise in CV risk:4
Footnotes
An observational study from the Stockholm CREAtinine Measurements (SCREAM) project included 84,399 adults with ASCVD (2007 to 2021). It assessed baseline hsCRP levels and their association with adverse cardiovascular outcomes and healthcare use. Regression models evaluated determinants and outcomes associated with elevated hsCRP (≥2 mg/L).4
MACE was a composite of hospitalization for myocardial infarction, stroke, or all-cause death.4
ASCVD was defined as receiving a diagnosis of coronary, cerebrovascular, or peripheral artery disease.4
A collaborative analysis of three global trials involving 31,245 patients with, or at high risk for, ASCVD receiving contemporary statins showed that CV inflammation was an independent predictor of MACE, CV death, and all-cause death, regardless of low-density lipoprotein cholesterol (LDL-C).1
Footnotes
A collaborative analysis of the multinational PROMINENT, REDUCE-IT, and STRENGTH trials (N=31,245) evaluated patients with or at high risk of ASCVD who were on statins and had moderately elevated triglycerides. PROMINENT and STRENGTH were neutral trials (pemafibrate vs placebo; omega-3 vs corn oil), while REDUCE-IT was a positive trial (icosapent ethyl vs mineral oil). Published between 2019–2022, these trials assessed residual inflammatory and cholesterol risk using hsCRP and LDL-C as biomarkers.1
A randomized trial involving 5,522 patients with chronic coronary disease found that even in patients receiving standard lipid-lowering, antithrombotic, and blood pressure therapies, CV inflammation can continue to drive CV events.5
Footnotes
Low-Dose Colchicine (LoDoCo2) trial was a randomized, double-blind, placebo-controlled trial in 5,522 patients with chronic coronary disease, evaluating daily colchicine vs placebo. The primary endpoint was a composite of CV death, spontaneous MI, ischemic stroke, or ischemia-driven coronary revascularization. Conducted from 2014 to 2020 at sites in Australia and the Netherlands.5
Sign up to receive the latest information about CV inflammation from Novo Nordisk
CV inflammation

CV inflammation:
An independent pathophysiological driver of ASCVD6
CV inflammation can drive each stage of atherogenesis in CVD6
- Development of endothelial cell dysfunction
- Plaque formation and progression
- Eventual plaque rupture
CV Inflammation can drive each stage of atherosclerotic disease6
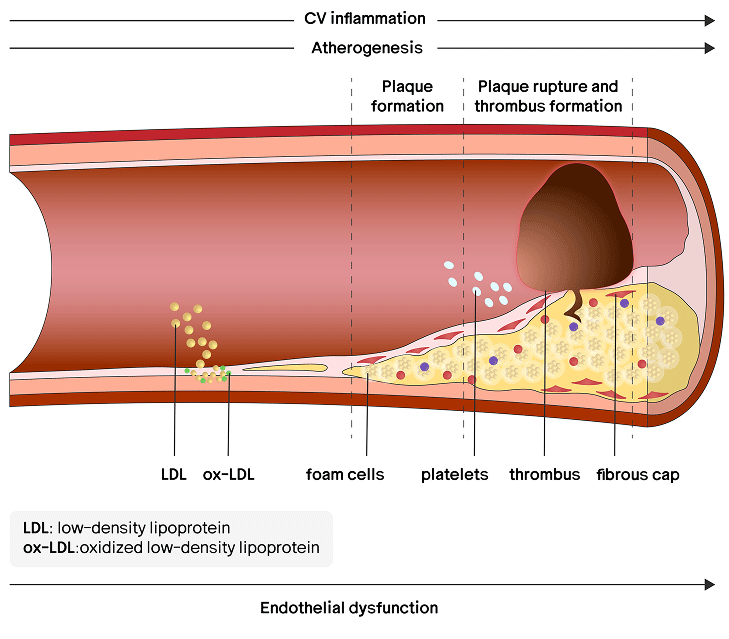
Based on Alfaddagh A et al. Am J Prev Cardiol. 2020; 4: 100130.
What role do you think CV inflammation plays in your patients with ASCVD?
(Select the option that best reflects your opinion)

I understand the role of CV inflammation, but it does not influence my management strategies

It is a risk-amplifier that causes me to treat other risk factors more aggressively

It is a key risk factor, and I am interested in learning about additional measures to help manage outcomes
I understand the role of CV inflammation, but it does not influence my management strategies

I understand the role of CV inflammation, but it does not influence my management strategies
It is a risk-amplifier that causes me to treat other risk factors more aggressively

It is a risk-amplifier that causes me to treat other risk factors more aggressively
It is a key risk factor, and I am interested in learning about additional measures to help manage outcomes

It is a key risk factor, and I am interested in learning about additional measures to help manage outcomes
Based on a multinational, randomized trial of 13,970 statin-intolerant participants, CV inflammation is an independent CV risk factor that predicts future CV events and is additive to the effects of traditional risk factors.3
Footnotes
The multinational CLEAR-Outcomes (Cholesterol Lowering via Bempedoic Acid, an ACL-Inhibiting Regimen Outcomes Trial) randomized 13,970 statin-intolerant participants with LDL-C >100 mg/dL to bempedoic acid or placebo and monitored CV events (myocardial infarction, stroke, coronary revascularization, or CV death) and all-cause mortality between December 2016 and August 2019. Baseline hsCRP and LDL-C quartiles were analyzed as predictors of adverse outcomes, adjusted for traditional risk factors and treatment.3
hsCRP Testing
hsCRP:
Exposing the inflammatory threat in CVD7–9
hsCRP is a key biomarker in assessing inflammatory CV risk.7–9
Collaborative analysis of three global trials found1:
Among 31,245 statin-treated patients from the PROMINENT, REDUCE-IT, and STRENGTH trials residual inflammatory CV risk, as measured by hsCRP, was significantly associated with CV death.1

Patients in the highest hsCRP quartile (>4.2 to >4.8 mg/L) had over 2.7x the risk of CV death compared to those in the lowest quartile (<1.1 to <1.2 mg/L) (adjusted hazard ratio 2.68, 95% confidence interval 2.22–3.23; p < 0.0001).1
Footnotes
A collaborative analysis of the multinational PROMINENT, REDUCE-IT, and STRENGTH trials (N=31,245) evaluated patients with or at high risk of ASCVD who were on statins and had moderately elevated triglycerides. PROMINENT and STRENGTH were neutral trials (pemafibrate vs placebo; omega-3 vs corn oil), while REDUCE-IT was a positive trial (icosapent ethyl vs mineral oil). Published between 2019–2022, these trials assessed residual inflammatory and cholesterol risk using hsCRP and LDL-C as biomarkers.1
hsCRP is a marker that can expose the inflammatory threat accelerating atherosclerosis in your patients with CV comorbidities.7
Sign up to receive the latest information about CV inflammation from Novo Nordisk.
FAQs

CV inflammation is an inflammatory response that, if unaddressed, can contribute to plaque destabilization and CV conditions like atherosclerosis and heart failure.2
Inflammatory CV risk is the risk indicated by hsCRP levels ≥2mg/L and is commonly referred to in literature as ‘inflammatory risk’.1,3
An observational study of 84,399 adults with ASCVD in the Stockholm CREAtinine Measurements (SCREAM) project showed that nearly 60% of patients with ASCVD have measurable inflammation (hsCRP ≥2 mg/L).4
CV inflammation can be detected using an hsCRP test, which is a key biomarker in assessing inflammatory CV risk.7–9
Higher hsCRP levels (2 mg/L or more) indicate greater inflammatory CV event risk, even if traditional CV risk factors are controlled.4,7-9
Clinical and pathological evidence suggests it is not just correlation. CV inflammation actively drives CV risk and may worsen CV outcomes.1,4
Standard care does not fully address inflammatory CV risk, leaving an opportunity for more comprehensive management.6
Abbreviations
AHA=American Heart Association; ASCVD=atherosclerotic cardiovascular disease; CV=cardiovascular; CVD=cardiovascular disease; HR=hazard ratio; hsCRP=high-sensitivity C-reactive protein; LDL-C=low-density lipoprotein cholesterol; MACE=major adverse cardiovascular event.
References
1. Ridker PM, Bhatt DL, Pradhan AD, et al. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomised trials. Lancet. 2023;401(10384):1293-1301. 2. Keller M, Mirakaj V, Koeppen M, Rosenberger P. Neuronal guidance proteins in cardiovascular inflammation. Basic Res Cardiol. 2021;116(1):6. Published 2021 Jan 29. doi:10.1007/s00395-021-00847-x. 3. Ridker PM, Lei L, Louie MJ, et al. Inflammation and Cholesterol as Predictors of Cardiovascular Events Among 13 970 Contemporary High-Risk Patients With Statin Intolerance. Circulation. 2024;149(1):28-35. doi:10.1161/CIRCULATIONAHA.123.066213. 4. Mazhar F, Faucon AL, Fu EL, et al. Systemic inflammation and health outcomes in patients receiving treatment for atherosclerotic cardiovascular disease. Eur Heart J. 2024;45(44):4719-4730. 5. Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020;383(19):1838-1847. 6. Alfaddagh A, Martin SS, Leucker TM, et al. Inflammation and cardiovascular disease: from mechanisms to therapeutics. Am J Prev Cardiol. 2020;4:100130. 7. Liuzzo G, Ridker PM. Universal screening for hsCRP in patients with atherosclerotic disease: a major therapeutic opportunity. Eur Heart J. 2024;45(44):4731-4733. doi:10.1093/eurheartj/ehae565. 8. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678. 9. Kamath DY, Xavier D, Sigamani A, Pais P. High sensitivity C-reactive protein (hsCRP) & cardiovascular disease: an Indian perspective. Indian J Med Res. 2015;142(3):261-268. doi:10.4103/0971-5916.166582.